Rural hospitals are discovering virtual contrast supervision can solve their radiologist shortage crisis and improve patient outcomes, but implementation success depends on meeting specific regulatory requirements. Here’s what makes a difference.
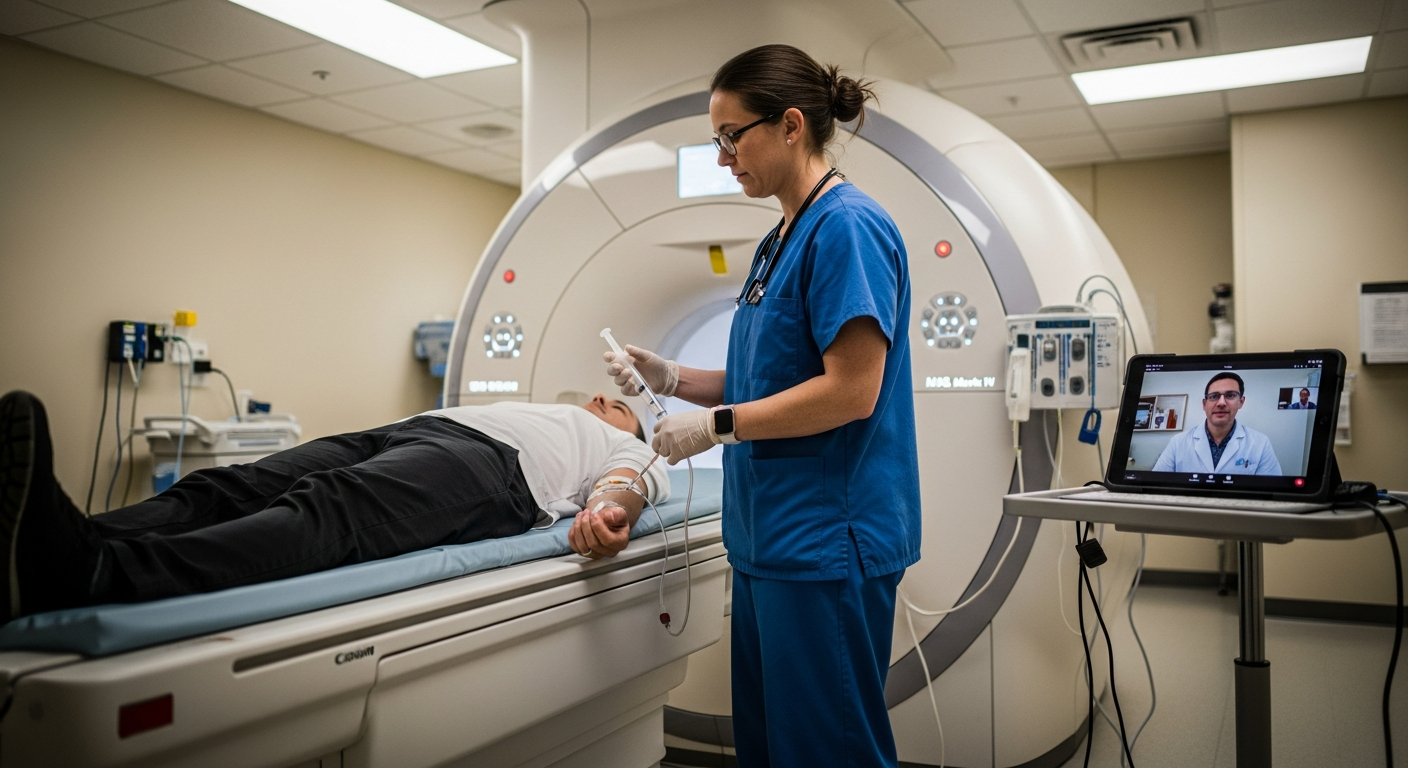
Rural hospitals across America face an ongoing crisis: radiologist shortages that limit patient access to critical imaging services. When contrast-enhanced procedures require on-site physician supervision, patients in remote areas often face delays, transfers to distant facilities, or postponed care. Virtual contrast supervision has emerged as a transformative solution, but many hospital administrators wonder if it truly works in practice.
The critical question remains: Will it really make a difference in rural settings, and if so, how?
The evidence is clear: virtual contrast supervision delivers measurable results for rural hospitals. Providers like ContrastConnect manage over 55,000 monthly exams and maintain a record of zero missed responses across urban and rural networks. Early forays into virtual contrast supervision are showing promising results for patients, physicians, and outpatient imaging centers serving rural communities. Hospitals implementing virtual supervision are seeing fewer staffing shortages, better equipment utilization, lower staff turnover, and improved patient care.
Virtual supervision enables rural hospitals to maintain service lines even with physician shortages, building long-term care capacity without overextending resources. Patients who previously faced transfers to urban facilities can now receive timely contrast-enhanced procedures locally, reducing both costs and treatment delays.
Regulatory support for virtual contrast supervision has never been stronger. Two significant developments in 2025 and 2026 solidify this technology as a permanent healthcare solution rather than a temporary emergency measure.
The Centers for Medicare & Medicaid Services (CMS) has finalized a rule to allow virtual direct supervision starting January 1, 2026, permanently. This decision extends the flexibility introduced initially during the COVID-19 public health emergency, providing rural hospitals with a compliant, long-term solution for managing staffing shortages.
The permanent approval means rural hospitals can invest confidently in virtual supervision infrastructure without worrying about policy reversals. CMS recognizes that real-time audio and video technology can effectively replace physical presence for many supervised procedures, including contrast administration.
The American College of Radiology has been a vocal advocate for permanent virtual supervision policies. The ACR emphasizes that virtual supervision improves patient access and reduces healthcare costs when specific guidelines are followed. Their updated guidelines provide detailed specifications for conducting remote contrast supervision, including protocols for technologist training, supervision availability, documentation, and emergency escalation procedures.
This professional backing gives rural hospital administrators confidence that virtual supervision aligns with industry best practices and maintains the highest safety standards for patients.
Rural hospitals face unique operational challenges that virtual supervision directly addresses. Understanding these benefits helps administrators evaluate whether this technology fits their facility's needs.
The radiologist shortage hits rural areas hardest. Many rural hospitals struggle to recruit physicians willing to relocate to their region, where imaging departments often go months without adequate coverage. Virtual supervision opens access to a much larger pool of qualified radiologists who can provide remote oversight without relocating.
When rural hospitals cannot perform contrast-enhanced procedures due to supervision requirements, patients must transfer to larger facilities hours away. These transfers create financial strain for families, delay treatment, and reduce hospital revenue. Virtual supervision eliminates this cascade of problems by enabling local care delivery.
Telehealth services, including virtual supervision, allow rural healthcare providers to offer quality healthcare services locally and at significantly lower costs than urban alternatives. Patients receive faster care closer to home, improving both outcomes and satisfaction.
Virtual supervision can reduce imaging center operational costs significantly, depending on facility size and existing staffing models. The technology eliminates expensive on-call arrangements, reduces the need for locum tenens coverage, and allows for more flexible scheduling and extended operating hours.
Improved resource allocation means radiologists can focus on diagnostic reading rather than travel time, increasing overall productivity. Rural hospitals often see immediate improvements in both cost management and service availability.
Successful virtual supervision implementation requires careful planning and attention to regulatory requirements. These best practices help ensure smooth deployment and ongoing compliance.
The technology platform must support live audio and video interactions while automating documentation and preserving data for compliance reviews. Every supervision session should be logged, timestamped, and accessible for accreditation or CMS audits. Choose platforms specifically designed for healthcare environments with built-in security features and redundancies.
Integration with existing hospital information systems streamlines workflows and reduces administrative burden on staff. Look for solutions that connect seamlessly with PACS, EHR systems, and existing communication tools.
Remote workflows often shift more procedural responsibility to on-site technologists. Training prepares staff to recognize adverse reactions, communicate clearly with remote physicians, and handle emergencies according to established protocols. The ACR guidelines provide specific requirements for technologist preparation in virtual supervision environments.
Ongoing education ensures technologists stay current with protocol changes and maintain confidence in remote procedures. Regular competency assessments help identify areas where additional training may be needed.
Clear escalation procedures are vital for patient safety during contrast reactions or other emergencies. All team members - both remote and on-site - must understand their roles and know how to initiate immediate care when needed.
Test these protocols regularly through simulation exercises to identify potential gaps and ensure smooth coordination between remote supervisors and on-site staff. Documentation of emergency procedures helps demonstrate compliance with safety standards.
Quarterly internal audits of supervision processes help ensure adherence to ACR and CMS standards while surfacing areas for improvement. These reviews should examine documentation practices, emergency response procedures, staff competency, and technology performance.
Proactive compliance monitoring helps avoid issues before they arise and demonstrates an ongoing commitment to quality patient care. Regular reviews also help identify opportunities to optimize workflows and improve efficiency.
The question isn't whether virtual contrast supervision works at rural hospitals - the evidence clearly shows it does. The real question is how quickly rural hospitals can implement this technology to serve their communities better. With permanent regulatory approval, professional organization support, and proven operational benefits, virtual supervision represents the future of rural imaging services.
