Starting January 2026, CMS will permanently allow direct supervision via real-time audio/video for applicable services. That shift can help outpatient imaging centers build more resilient coverage models—without changing the need for on-site readiness and contrast safety protocols.
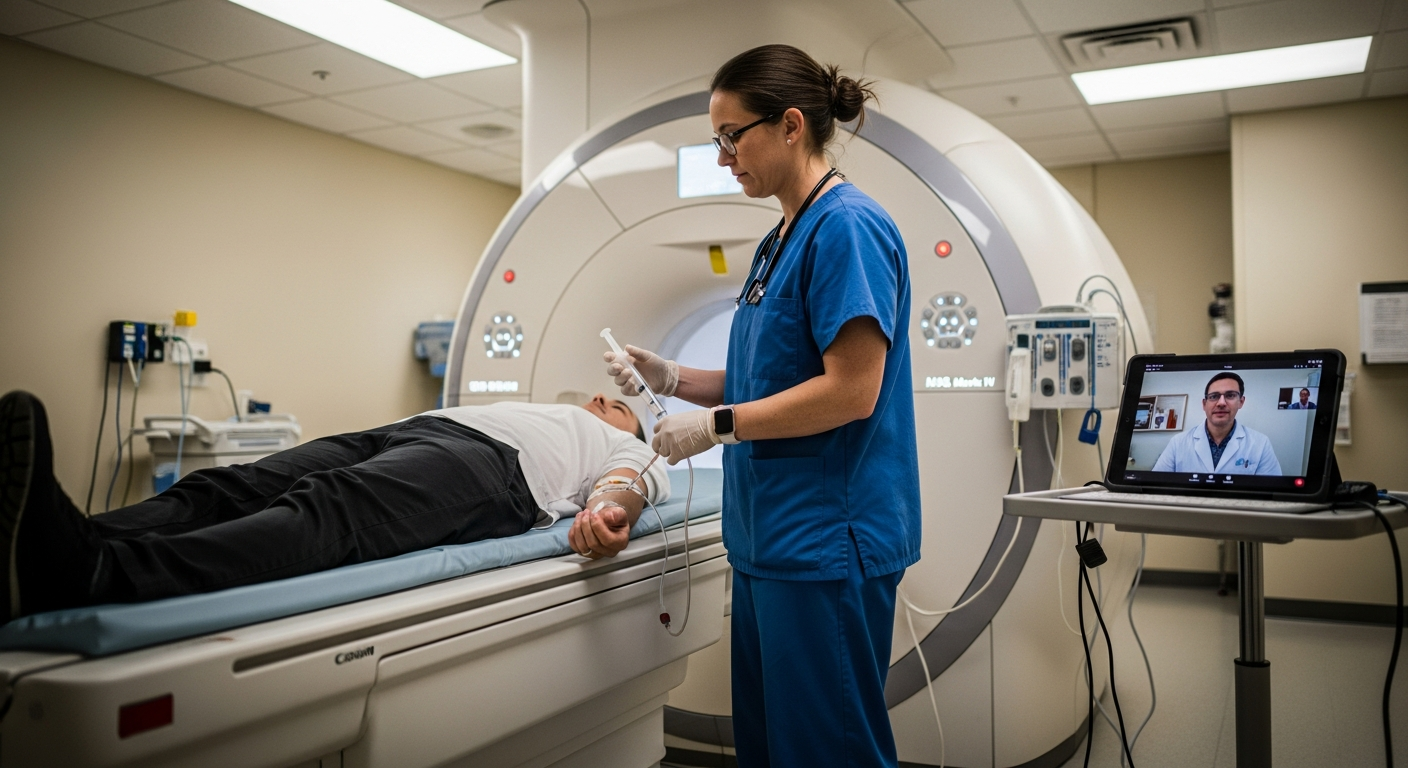
The Centers for Medicare & Medicaid Services (CMS) has finalized a permanent update to how "direct supervision" can be provided under the Medicare Physician Fee Schedule. Starting January 1, 2026, CMS is permanently adopting a definition of direct supervision that allows the physician or supervising practitioner to provide such supervision through real-time audio and visual interactive telecommunications (excluding audio-only) for applicable services—including diagnostic tests under § 410.32.
For outpatient imaging facilities, this shift provides much-needed regulatory clarity. It also supports long-term planning for virtual coverage models—particularly in environments where maintaining consistent on-site physician coverage is operationally complex.
Outpatient imaging centers live and die by operational reliability. Even small supervision gaps can ripple into delayed starts, patient dissatisfaction, overtime, and lost revenue. Virtual coverage can reduce those bottlenecks by making supervision more resilient.
Many imaging networks operate multiple sites with uneven daily volumes. Requiring a supervising physician physically on-site at every location can be expensive and inefficient—especially when one site is slow while another is backed up. Virtual coverage helps centralize supervision so organizations can align coverage with demand (where allowed), rather than with geography.
Offering early mornings, evenings, and weekends can improve access and scanner utilization—but only if supervision coverage is reliable. Virtual coverage can support extended hours without forcing facilities into last-minute locums coverage or schedule reductions when an on-site supervisor isn't available.
When direct supervision coverage falls through, contrast-enhanced studies are often the first to be rescheduled. Virtual coverage can provide dependable backup and reduce "day-of" cancellations that disrupt operations and frustrate patients.
Virtual coverage is not "less supervision." It is a different way to meet supervision expectations—one that must be implemented with clear guardrails.
CMS's finalized policy explicitly excludes audio-only technology. Your program should support real-time audio and video communication that allows the supervising physician/practitioner to remain immediately available and intervene when necessary.
ACR's position is clear: direct supervision is required whenever contrast material is administered. ACR notes this direct supervision requirement can be met by an on-site radiologist, other physician, or qualified licensed practitioner (as permitted by law and policy). It also states that virtual supervision of qualified on-site personnel should only be performed by a physician, with bi-directional communication, and that only one level of virtual supervision should occur.
Critically, ACR also emphasizes on-site staffing beyond the technologist: on-site personnel, in addition to the radiology technologist, must include at least one licensed practitioner with training and competencies that include patient assessment, medication administration (including IV medications such as epinephrine), and emergency interventions, consistent with state law and facility policy.
In other words, the operational model can be virtual—but the safety model must remain real and ready on-site.
A compliant virtual coverage program should produce clear records that show:
This matters not only for reimbursement integrity but also for audit readiness and risk management.
For outpatient imaging centers, the most helpful way to estimate impact is to translate virtual coverage into three buckets:
Start with disruption. If a site currently delays or reschedules contrast cases when coverage is unavailable, quantify the number of affected appointments per week and the average downstream impact: rebooking time, overtime to "catch up," and lost margin when patients go elsewhere. Even modest disruption (for example, a few contrast slots per day) can create cascading delays across CT/MR, front desk, and nursing.
Next, labor efficiency. Many centers cover sporadic contrast needs by "overstaffing for peaks" (keeping a supervising clinician available for low-frequency events). Virtual coverage can convert that fixed cost into a variable one—aligning coverage to actual scan volume and hours of operation—while still supporting real-time communication and escalation pathways.
Finally, protect throughput. When contrast studies are blocked, non-contrast substitutions, longer room turnover, and schedule gaps reduce utilization of high-cost scanners. Estimate current scanner utilization (scheduled vs. completed scans), then model a conservative improvement (e.g., reclaiming a small percentage of previously lost slots). The goal isn't a universal ROI claim—it's a repeatable worksheet your team can defend with internal data, payer mix, and compliance requirements.
Federal policy isn't the only consideration. State supervision and scope-of-practice rules can be more specific.
For example, California's AB 460 (effective January 1, 2026) amends the Radiologic Technology Act to permit certified radiologic technologists to perform venipuncture for contrast materials under "direct supervision" that can be met either by physical presence or by remote presence via real-time audio/video communication, with additional safety protocol expectations.
For multi-state imaging networks, this is precisely why implementation should start with a state-by-state compliance review.
As outpatient imaging networks evaluate virtual coverage models for 2026 and beyond, the key is not just "having video." It's building a program that aligns with CMS rules, ACR expectations, and state requirements—while improving operational reliability across dozens (or hundreds) of sites.
For imaging centers, this translates into working with reliable virtual contrast supervision providers to receive compliance support, consistent coverage, clear escalation pathways, and audit-ready documentation—so facilities can reduce cancellations, extend hours, and streamline daily operations without relying on inefficient on-site coverage models.
