Testosterone levels start dropping 1% yearly after 30, yet many younger men dismiss fatigue, muscle loss, and mood changes as “just stress.” But when do these symptoms actually signal something treatable—and what are your real options beyond hormone replacement?
Low testosterone isn't just an older man's concern. As men enter their thirties, declining hormone levels can significantly impact quality of life, energy, and overall wellbeing. Understanding when to seek help and what treatment options exist can make the difference between struggling through symptoms and reclaiming vitality.
The numbers tell a compelling story about testosterone decline in younger men. Testosterone levels generally peak during adolescence and early adulthood, then begin their steady descent by approximately 1% per year after age 30 or 40. This gradual decline means that by age 35, many men have already experienced a 5-10% reduction from their peak levels.
What's particularly striking is the surge in testosterone replacement therapy use among younger demographics. Statistical trends show TRT use increased fourfold from 2003 to 2013 for men aged 18 to 45, compared to a threefold increase in older men.
The American Urology Association defines low testosterone as less than 300 ng/dL, though some healthcare providers may consider levels below 250 ng/dL as low, with diagnosis also considering symptoms. Many men experience symptoms even when their levels fall within the lower range of "normal." This creates a grey area where younger men might dismiss legitimate concerns, attributing fatigue and mood changes to work stress or lifestyle factors rather than recognising potential hormonal imbalances.
Early detection of low testosterone symptoms can prevent years of diminished quality of life. The challenge lies in recognising that seemingly unrelated issues might stem from declining hormone levels.
The physical manifestations of low testosterone often develop gradually, making them easy to overlook. Decreased muscle mass and increased body fat represent two of the most significant changes. Testosterone supports muscle mass and aids in red blood cell production necessary for oxygen delivery. It also supports mitochondrial function responsible for energy production at the cellular level.
Persistent fatigue stands out as one of the most reported symptoms, often accompanied by reduced exercise capacity and longer recovery times. Men might notice they can't maintain previous workout intensities or that building muscle becomes increasingly difficult despite consistent training. Sleep disturbances frequently compound these issues, creating a cycle where poor sleep further impacts hormone production.
Low testosterone's impact on mental health deserves serious attention. Depression, irritability, and brain fog commonly accompany declining testosterone levels, though these symptoms are often attributed to external stressors rather than hormonal changes.
Concentration difficulties and memory problems can affect work performance and personal relationships. Many men describe feeling "off" or lacking their usual drive and motivation, experiencing what some describe as an emotional flatness that affects their engagement with previously enjoyable activities.
Reduced sex drive and erectile dysfunction represent perhaps the most recognisable symptoms of low testosterone. These changes can strain relationships and further impact mental health, creating a compound effect that extends beyond physical symptoms.
Sexual health issues often serve as the catalyst for men to seek medical attention, as they directly impact quality of life and relationship satisfaction. However, these symptoms rarely occur in isolation and typically accompany other physical and mental changes.
Understanding the root causes of low testosterone helps determine appropriate treatment approaches and whether the condition might be reversible through lifestyle changes or requires medical intervention.
Modern lifestyle factors play a significant role in early testosterone decline. Chronic stress elevates cortisol levels, which directly suppresses testosterone production. Poor sleep quality compounds this effect, as a significant part of testosterone production happens during deep sleep.
Obesity creates a particularly problematic cycle, as excess body fat increases aromatase enzyme activity, converting testosterone to oestrogen. Meanwhile, sedentary behaviour reduces the natural testosterone-boosting effects of resistance training and physical activity. Dietary factors, including excessive alcohol consumption and highly processed foods, further contribute to hormonal imbalance.
Several medical conditions can cause low testosterone in younger men. Damage to testicles from injury or infection, chemotherapy or radiation treatments, and pituitary gland disorders represent more serious underlying causes requiring medical intervention.
Anabolic steroid use stands out as one of the most common causes of low testosterone in young men, as it suppresses natural hormone production that may not fully recover after cessation. Other medications, including opioids and certain antidepressants, can also impact testosterone levels. Autoimmune diseases and genetic conditions like Klinefelter syndrome represent less common but significant causes.
Proper testing forms the foundation of any testosterone treatment plan, yet many men don't understand when and how to get tested effectively.
Testosterone testing requires specific timing and conditions for accurate results. Total testosterone levels naturally fluctuate throughout the day, typically peaking in the morning. Tests should be conducted between 7 AM and 10 AM for the most reliable readings.
Multiple tests are often necessary, as testosterone levels can vary significantly from day to day based on sleep, stress, and other factors. A single low reading doesn't necessarily indicate a chronic condition, which is why healthcare providers typically require two or more low readings before considering treatment.
Several different testosterone measurements provide insights into hormone status. Total testosterone measures the complete amount of hormone in the blood, while free testosterone represents the amount available for use by body tissues. Some men have normal total testosterone but low free testosterone due to high levels of sex hormone-binding globulin (SHBG).
Bioavailable testosterone, which includes both free testosterone and testosterone weakly bound to albumin, often provides the most clinically relevant information. Understanding these distinctions helps explain why some men with "normal" total testosterone still experience symptoms and may benefit from treatment.
Testosterone replacement therapy isn't the only option for addressing low testosterone symptoms. A thorough approach often yields the best results.
Strategic lifestyle changes can significantly impact testosterone levels, particularly when deficiency stems from modifiable factors. Resistance training, especially compound movements like squats and deadlifts, provides one of the most effective natural testosterone boosts. Adequate sleep - ideally 7-9 hours nightly - supports natural hormone production cycles.
Dietary interventions focusing on adequate healthy fats, sufficient protein, and strategic micronutrient supplementation can support hormone production. Weight loss in overweight men often results in substantial testosterone increases, as reducing body fat decreases aromatase activity and improves insulin sensitivity.
Treating underlying medical conditions often resolves testosterone deficiency without requiring hormone replacement. Managing diabetes improves insulin sensitivity and hormone production, while addressing sleep apnea can dramatically improve testosterone levels and energy.
Thyroid disorders, vitamin D deficiency, and chronic inflammatory conditions all impact testosterone production and respond well to targeted treatment. This underscores the importance of thorough medical evaluation rather than jumping directly to hormone replacement.
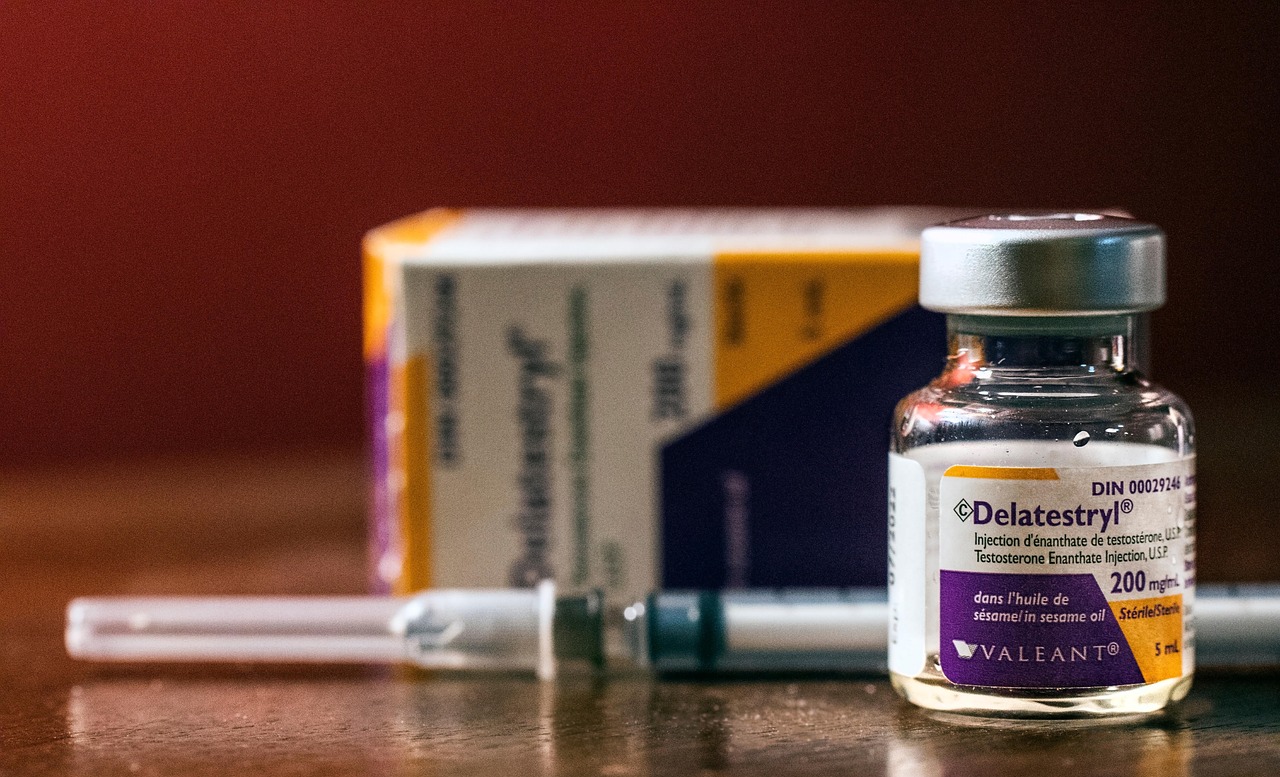
When lifestyle modifications and underlying condition treatment don't adequately address symptoms, testosterone replacement therapy becomes a viable option. Modern TRT options include injections, gels, patches, and pellets, each with distinct advantages and considerations.
TRT can improve sexual function, lean body mass, bone mineral density, mood, energy levels, and overall sense of wellbeing. However, treatment requires ongoing medical supervision and regular monitoring to ensure safety and effectiveness while minimising potential side effects.
Any medical treatment requires careful consideration of potential benefits versus risks, and testosterone therapy is no exception.
Research demonstrates that testosterone replacement therapy can effectively improve sexual function, including libido and erectile function, in men with confirmed low testosterone. Studies show significant improvements in lean body mass and strength, particularly when combined with resistance training.
Energy improvements often represent the most immediately noticeable benefit, as testosterone replacement may be effective in reversing age-dependent body composition changes and associated morbidity. Bone mineral density improvements provide long-term skeletal health benefits, while mood and cognitive function improvements enhance quality of life.
Testosterone therapy carries several potential risks that require careful consideration. Common side effects include acne, sleep apnea worsening, and prostate enlargement. More serious concerns include increased red blood cell production, which can increase blood clot risk, and potential cardiovascular effects, though research on heart disease risk remains inconclusive.
Fertility represents a significant concern for younger men, as testosterone therapy can suppress sperm production and potentially impact future fertility. Some studies suggest that TRT can increase the risk of heart disease, though more research is needed to fully understand these relationships.
The decision to pursue testosterone evaluation and potential treatment requires professional medical guidance. Self-diagnosis based on symptoms alone can lead to inappropriate treatment or missed underlying conditions that require different interventions.
A thorough evaluation includes detailed symptom assessment, physical examination, and appropriate laboratory testing. This approach helps distinguish between testosterone deficiency and other conditions with similar symptoms, ensuring men receive the most appropriate treatment for their specific situation.
Quality of life improvements from proper testosterone management can be substantial, but only when treatment is medically appropriate and professionally supervised. The investment in proper evaluation pays dividends in both immediate symptom relief and long-term health outcomes.
Seeking professional medical advice for testosterone evaluation and treatment is the first step toward addressing potential hormone deficiency and improving overall health and wellbeing.
