Non-communicable diseases now account for nearly three-quarters of global deaths. In low- and middle-income countries, where health systems are often under strain, primary care could be the key to saving millions of lives and extending average life expectancy.
Non-communicable diseases (NCDs) have become the leading cause of death worldwide, responsible for 41 million deaths each year. According to the World Bank and the World Health Organization, 74% of all deaths are linked to NCDs, and a striking 82% of premature deaths occur in low- and middle-income countries (LMICs).
This is more than just a statistic—it reflects a major epidemiological transition. Infectious diseases, maternal complications, and neonatal causes are no longer the primary threats in many regions. Instead, long-term conditions like hypertension, diabetes, cancer, and respiratory illness dominate the health landscape.
The challenge? Many LMIC health systems are still designed to treat acute or episodic conditions. Preventive care, early screening, treatment, and long-term management of NCDs are often missing. The result is millions living undiagnosed, untreated, or forced to travel long distances to access basic care.
The World Health Organization (WHO) estimates that strengthening primary health care in LMICs could prevent up to 60 million deaths by 2030 and increase average life expectancy by 3.7 years. Yet fewer than half of these countries currently have robust NCD interventions integrated into their primary care systems.
Evidence-based tools exist, but implementation lags. The WHO's Package of Essential Non-Communicable Disease Interventions can help curb NCD rates, but countries often face resource constraints, political hurdles, and workforce shortages.
Digital health solutions, highlighted in Nature (2023), also remain underused. Only half of WHO's recommended digital categories for NCD care have been deployed in LMICs so far, despite promising results for patient engagement and health service efficiency.
Workforce shortages, limited access to essential medicines, and weak system responsiveness remain critical obstacles. Data gaps make it even harder to design and evaluate reforms.
There are, however, encouraging signs. Community-based models, integration of NCD services into primary care, and task-sharing with non-physician health workers are showing promise. WHO's PRIMASYS initiative has also documented best practices across 20 countries, offering insights into what works and what still needs scaling.
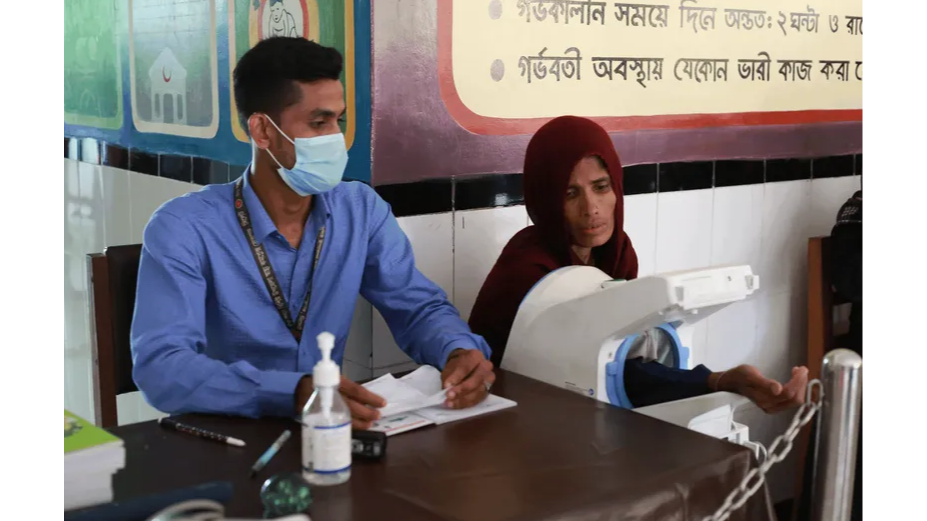
In India, for example, a nationwide plan is underway to provide treatment for 75 million people with hypertension and diabetes by 2025, with advocacy-supported initiatives built directly into federal health programs. In Bangladesh, adding essential hypertension medicines to rural clinic drug lists has made treatment accessible to low-income patients who would otherwise lose hours of wages traveling for medication.
These are not isolated wins—they are signals of what is possible when policy shifts, resources align, and advocacy brings NCDs into the primary care spotlight.
Experts point out that sustainable change often comes through policy. As one health advocacy leader explains: "Policy changes at national and subnational levels can shift population health outcomes and improve social norms. A systematic approach helps partners build sustainable movements that deliver lasting benefits."
Organizations such as the Global Health Advocacy Incubator work with local civil society groups, governments, and media to strengthen these advocacy efforts. By building technical capacity and pushing for policy reforms, they help ensure that long-term investment, trained healthcare workers, and affordable access to medicines remain priorities.
Strong primary care systems are not just a backbone of health—they are a lifeline for millions facing chronic conditions in LMICs. When prevention, screening, and long-term management are brought closer to communities, the gains are profound: fewer premature deaths, healthier lives, and more resilient systems.
If you're exploring how policy and advocacy can help close NCD treatment gaps, looking to organizations like the Global Health Advocacy Incubator offers valuable insights into strategies that work.
