Healthcare’s radiologist shortage is set to hit 42,000 by 2033, but CMS just made a game-changing policy permanent starting January 2026. One remote specialist can now oversee multiple facilities simultaneously—but there’s a crucial technology requirement most don’t know about.
Healthcare faces an unprecedented crisis as radiology departments nationwide struggle with severe staffing shortages. More than 80% of health systems report gaps in their radiology departments, creating a healthcare emergency that threatens timely patient diagnosis and treatment. The situation continues deteriorating as the number of imaging studies increases by up to 5% per year, while the number of radiology residency positions only increases by 2%, exacerbating the strain on the radiologist workforce.
This shortage hits particularly hard in underserved regions, where some areas have as few as 9 radiologists per 100,000 people. The disparity creates heavier workloads for remaining providers, contributing to burnout and early retirements that compound the problem. According to the Neiman Health Policy Institute, this radiologist shortage will likely persist until 2055 without corrective action.
The economic pressure intensifies these challenges. Understanding who can administer medications during contrast reactions becomes crucial as facilities seek efficient supervision solutions that maintain safety standards.
The Centers for Medicare and Medicaid Services has permanently adopted virtual direct supervision for diagnostic tests, effective January 1, 2026, recognizing its critical role in addressing healthcare access challenges. This policy change makes permanent the COVID-19-era flexibility that allowed remote oversight of medical procedures.
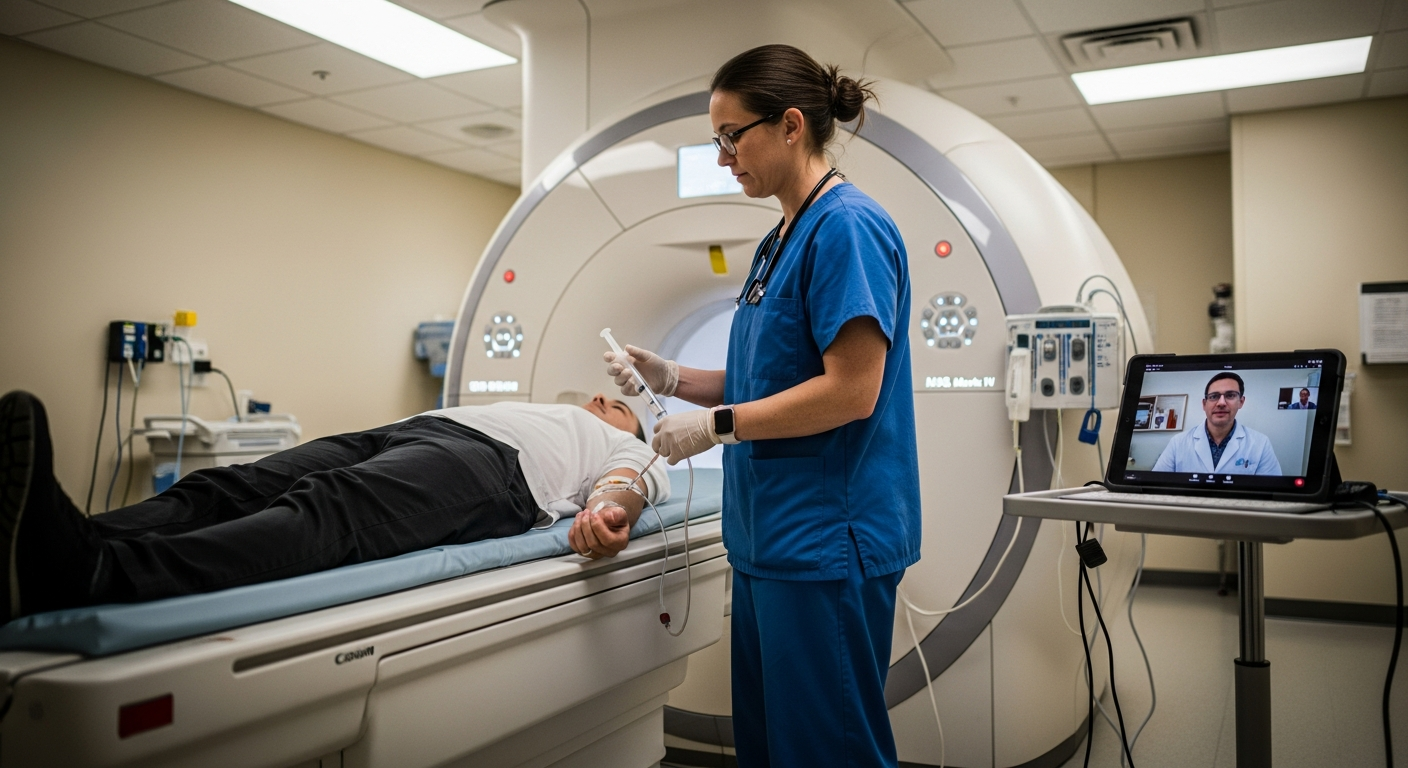
CMS altered the definition of "direct supervision" to permit supervising providers to meet presence and "immediate availability" requirements through real-time audio and visual interactive telecommunications. This technology-enabled approach maintains safety standards while eliminating the need for physical presence during every procedure. The American College of Radiology formally urged CMS to make virtual supervision permanent, emphasizing its benefits in improving patient access and reducing healthcare costs without compromising safety.
The permanent policy specifically covers Level 2 diagnostic tests and other services requiring direct supervision under existing CMS regulations. Supervising physicians and non-physician practitioners can now satisfy presence requirements through secure audiovisual connections throughout test performance. However, CMS expressly excluded services with 010 or 090 global surgery indicators, which represent minor and major procedures requiring extended post-operative care periods.
Virtual supervision transforms operational capacity for imaging centers by allowing radiologists to provide oversight across multiple facilities simultaneously. This capability addresses geographic barriers and staffing limitations that previously restricted service availability, particularly in rural or underserved areas.
Advanced telecommunications technology enables one radiologist to monitor procedures at several locations, dramatically improving resource efficiency. This multi-site coverage model reduces per-facility staffing costs while ensuring continuous expert oversight. Imaging networks benefit from centralized specialist expertise without maintaining full-time radiologists at every location.
Remote radiologists specializing in virtual supervision often manage more contrast reactions weekly than typical on-site providers see in months. This concentrated experience translates to superior recognition of complications and more effective intervention strategies. A survey by the RBMA (Radiology Business Management Association) reported that approximately 30% of imaging centers experienced faster response times with virtual supervision compared to on-site models, as specialized remote providers maintain constant readiness for emergency situations.
Extended operational hours become feasible through virtual coverage, eliminating the prohibitive costs of maintaining on-site radiologist presence during off-peak times. Facilities can schedule contrast studies more flexibly, accommodate patient needs during evening and weekend hours, and handle volume surges without workflow disruptions. This flexibility particularly benefits multi-location imaging networks managing diverse scheduling demands.
Successful virtual supervision implementation depends on robust technology foundations and thorough staff preparation. Healthcare facilities must establish reliable systems that meet regulatory requirements while supporting seamless operational workflows.
Virtual supervision platforms must incorporate security features including end-to-end encryption, secure authentication protocols, and detailed audit trails. These systems require high-definition cameras with appropriate positioning, clear audio systems for two-way communication, and reliable high-speed internet connectivity with backup connections. Integration capabilities with existing Picture Archiving and Communication Systems and Electronic Health Records ensure seamless documentation flow without duplicate data entry.
Radiologic technologists need specialized instruction on equipment operation, communication protocols with remote radiologists, and emergency response procedures. Training programs should cover platform navigation, troubleshooting common technical issues, and maintaining effective communication during procedures. Regular refresher sessions keep skills current and ensure consistent performance across all staff members as technology and protocols evolve.
Modern virtual supervision platforms generate documentation automatically, reducing administrative burden while ensuring complete regulatory compliance. These systems create audit-ready records that support quality assurance reviews and regulatory inspections.
Documentation systems include timestamp records of supervision sessions, interaction logs between radiologists and technologists, and detailed reports of any interventions or guidance provided. Pre-configured templates ensure all required information is captured consistently, while customizable workflows accommodate facility-specific protocols and preferences. This automated approach eliminates manual documentation errors and reduces administrative time requirements.
Virtual supervision platforms accommodate varying state regulations and professional organization requirements through configurable compliance modules. These systems monitor regulatory changes and update documentation requirements automatically, ensuring facilities remain compliant as regulations evolve. Integration with state-specific protocols and professional guidelines provides coverage for multi-state imaging networks.
Implementation of virtual contrast supervision generates significant operational savings through improved resource utilization and reduced staffing overhead. Facilities report substantial cost reductions in evening, weekend, and holiday coverage while maintaining or improving service quality and patient safety outcomes.
The economic benefits extend beyond direct staffing costs to include reduced procedure cancellations, extended facility utilization, and improved scheduling flexibility. These operational improvements translate to enhanced revenue potential while addressing the critical shortage of radiologist expertise. Healthcare administrators find virtual supervision provides a sustainable solution for managing staffing challenges without compromising patient care standards.
For imaging centers seeking reliable virtual contrast supervision solutions, specialized providers can offer CMS-compliant remote oversight with experienced radiologists.
